Category: Medicine, Health
Two More Vaccines and a Drug join India’s Fight against COVID
30, Dec 2021

Why in News?
- India has recently approved two more vaccines under emergency use authorisation and an antiviral drug, Molnupiravir.
About the News:
- Currently, India uses Covishield, Covaxin and Sputnik V in its vaccination programme.
- Corbevax is co-developed by Biological E, Baylor College of Medicine in Houston, United States, and American company Dynavax Technologies.
- Covovax is produced by the Serum Institute of India under licence from Novavax, a U.S.-based biotechnology company.
- Covovax has been approved by the World Health Organisation (WHO) under its Emergency Use Listing and, therefore, will also be available globally as part of the COVAX initiative to ensure that at least 40% of world is vaccinated on priority.
Regular procedure for Drug Approval:
- Vaccines and medicines, and even diagnostic tests and medical devices, require the approval of a regulatory authority before they can be administered.
- In India, the regulatory authority is the Central Drugs Standard Control Organisation (CDSCO).
- For vaccines and medicines, approval is granted after an assessment of their safety and Effectiveness, based on data from Trials.
About CDSCO:
- The Central Drugs Standard Control Organisation (CDSCO) under Directorate General of Health Services, Ministry of Health & Family Welfare, Government of India is the National Regulatory Authority (NRA) of India.
- Under the Drugs and Cosmetics Act, CDSCO is responsible for
- Approval of New Drugs
- Conduct of Clinical Trials
- Laying down the standards for Drugs
- Control over the quality of imported Drugs in the country and
- Coordination of the activities of State Drug Control Organizations by providing expert advice with a view to bring about the uniformity in the enforcement of the Drugs and Cosmetics Act.
- CDSCO along with state regulators is jointly responsible for grant of licenses of certain specialized categories of critical Drugs such as blood and blood products, Vaccine and Sera.
When can Emergency use Authorisation (EUA) be Granted?
- In the US, the Food and Drug Administration (FDA) grants EUA only after it has been determined that the “known and potential benefits outweigh the known and potential risks of the vaccine” (or medicine).
- This means that a EUA application can be considered only after sufficient efficacy data from phase 3 trials had been generated.
- A EUA cannot be granted solely on the basis of data from phase 1 or phase 2 trials.
What is the process of getting an Emergency use Authorisation in India?
- Experts and activists say India’s drug regulations do not have provisions for a EUA, and the process for receiving one is not clearly defined or consistent.
- Despite this, CDSCO has been granting emergency or restricted emergency approvals to COVID-19 drugs during this pandemic for Remdesivir and favipiravir.
- Already it has granted permission for Covaxin, Covishield and Sputnik V. Check alcohol rehab west palm.
Is there a risk in using a Product that has only been Granted a EUA?
- Now the public has to be informed that a product has only been granted an EUA and not Full Approval.
- In the case of a Covid-19 vaccine, for example, people have to be informed about the known and potential benefits and risks, and the “extent to which such benefits or risks are unknown”, and that they have a right to refuse the Vaccine.
NEGLECTED TROPICAL DISEASE
31, Jan 2020
Why in News?
- January 30, 2020 is the First-Ever World Neglected Tropical Diseases Day(World NTD Day).
What is Neglected Tropical Disease?
- Neglected tropical diseases (NTDs) are a diverse group of tropical infections which are common in low-income populations in developing regions of Africa, Asia, and the Americas.
- They are caused by a variety of pathogens such as viruses, bacteria, protozoa and Helminths.
How these Diseases are Spread?
- Infections are caused by unsafe water, poor housing conditions and poor sanitation.
- Children are the most vulnerable to these diseases, which kill, impair or permanently disable millions of people every year, often resulting in life-long physical pain and social stigmatization.
How they can be Controlled?
- Many neglected tropical diseases can be prevented, eliminated or even eradicated with improved access to existing safe and cost-effective tools.
- Control relies on simple interventions that can be carried out by non-specialists — for example schoolteachers, village heads and local volunteers — in community-based preventive action.
Why are some Tropical Diseases called “Neglected”?
- The people who are most affected by these diseases are often the poorest populations, living in remote, rural areas, urban slums or Conflict Zones.
- Neglected tropical diseases persist under conditions of poverty and are concentrated almost exclusively in impoverished populations in the developing world.
What are the Lacking Features?
- A comprehensive policy to foster research and InnovationIn drug discovery, diagnostics, and vaccine development in neglected tropical diseases is lacking.
- While political intent and will are expressed in a few, Clear Operational Plans and Funding Mechanisms are not specified. Consequently, follow-up action is patchy or absent.
- No institutional mechanism exists at a national levelto identify gaps in neglected diseases research, set priorities, liaise with research institutions, or monitor research output.
- There is often no coordination between the various funding and research bodiesto prioritise the research agenda and Minimise Duplication.
What are the Challenges Faced?
- Lack of reliable statistics and unpronounceable names of diseases have all hampered efforts to bring them out of the shadows.
- Neglected tropical diseases affect more than 1 billion people, primarily poor populations living in tropical and subtropical climates.
- They are frequently clustered together geographically and individuals are often afflicted with more than one parasite or infection.
- More than 70% of countries and territories that report the presence of neglected tropical diseases are low-income or lower Middle-Income Economies.
Government Initiatives on Neglected Diseases:
- The National Health Policy (2017)sets an ambition to stimulate innovation to meet health needs and ensure that new drugs are affordable for those who need them most, but it does not specifically tackle neglected diseases.
- The National Policy on Treatment of Rare Diseases (2018)includes infectious tropical diseases and identifies a need to support research on treatments for rare diseases. It has not yet prioritised diseases and areas for research funding or how innovation would be supported.
Need of Hour:
- A Unified Programme on Neglected Diseases Encompassing Research and elimination measuresis likely to have a greater impact in prioritising the matter in the health agenda and streamlining efforts towards disease elimination.
- Creating an Enabling Environment for Research and Innovationwill be crucial if India is to achieve the target set in sustainable development goal 3.3 to end epidemics of neglected tropical diseases by 2030.
NATIONAL COMMISSION FOR INDIAN SYSTEM OF MEDICINE BILL, 2019
30, Jan 2020

Why in News?
- Cabinet approves proposal for official amendments in the National Commission for Indian System of Medicine (NCIM) Bill, 2019.
Highlights:
- The NCIM bill is aimed at bringing reforms in the medical education of the Indian medicine sector in lines with the National Medical Commission proposed for Allopathic system of medicine.
- The draft bill provides for the constitution of a National Commission with four autonomous boards entrusted with conducting overall education of Ayurveda under the Board of Ayurveda and Unani, Siddha and Sowarigpa under the Board of Unani, Siddha and Sowarigpa.
- The bill is currently pending in the Rajya Sabha.
- The Proposed Legislation Will:
- Ensure necessary regulatory reforms in the field of Indian System of Medicine education.
- Enable transparency and accountability for protecting the interest of the general public.
- The Commission will also promote the availability of affordable healthcare services in all parts of the country.
- The Commission has been structured to streamline the functions related to academic standards, evaluation, assessment and accreditation of educational institutions pertaining to the Indian System of Medicine.
- The main objective of establishing the NCIM is to promote equity by ensuring an adequate supply of quality medical professionals and enforce high ethical standards in all aspects of medical services in the Indian System of Medicine.
NATIONAL COMMISSION FOR HOMOEOPATHY BILL, 2019
30, Jan 2020

Why in News?
- Cabinet approves official amendments in the National Commission for Homoeopathy Bill, 2019.
Highlights:
- The Union Cabinet has given its approval to the official amendments in the National Commission for Homoeopathy Bill, 2019 for amending the Homoeopathy Central Council (HCC) Act, 1973. At present, the Bill is pending in Rajya Sabha.
- The Amendments intend to ensure necessary regulatory reforms in the field of Homoeopathy Education.
- They will also enable transparency and accountability for protecting the interests of the general public.
- The bill seeks the establishment of the National Commission for Homoeopathy, which will replace the current regulatory body for homoeopathy, the Homoeopathy Central Council.
- The Commission will promote the availability of affordable healthcare services in all parts of the country.
- The Homoeopathy Central Council (HCC) Act, 1973 was enacted for:
- The constitution of a Central Council of Homoeopathy for the regulation of education and practice of Homoeopathy.
- The maintenance of a Central Register of Homoeopathy and for matters connected therewith.
- The broad functions, constitution and regulation-making powers of the Council are identical to those of the Medical Council of India.
- While the Act provides a solid foundation for the growth of medical education and practice in Homoeopathy, various bottlenecks in the functioning of the Council have been experienced, which has resulted in serious detrimental effects on medical education as well as delivery of quality Homoeopathy Healthcare Services.
CORONAVIRUS
28, Jan 2020

Context:
- China is struggling to contain the spread of a new virus that has claimed at least six lives so far since 31st December. Almost 300 people have been hospitalised. Worryingly enough doctors have confirmed that the infection is spreading Rapidly Among Humans.
The Coronavirus Contagion:
- The Coronavirus outbreak has triggered memories of SARS or severe acute respiratory syndrome, which originated in China in 2002,
- By 2003 it infected more than 8,000 people and killed 774 in a pandemic that ripped through Asia.
- The present Coronavirus, was first detected in Wuhan city that has cancelled the upcoming Lunar New Year celebrations, where hundreds of thousands of people were expected to gather.
- Chinese doctors believe the disease is spreading far more easily than it was thought previously.
What Is a Coronavirus?
- Coronaviruses were first identified in the 1960s
- They get their name from their crown-like shape. Sometimes, but not often, a coronavirus can infect both animals and humans.
- Most coronaviruses spread the same way other cold-causing viruses do:
- Through infected people coughing and sneezing,
- By touching an infected person’s hands or face, or
- By touching things such as door knobs that infected people have touched.
- Almost everyone gets a coronavirus infection at least once in their life, most likely as a young child.
- In the United States, coronaviruses are more common in the fall and winter, but anyone can come down with a coronavirus infection at any time.
Common Human Coronaviruses:
- Common human coronaviruses, including types 229E, NL63, OC43, and HKU1, usually cause mild to moderate upper-respiratory tract illnesses, like the common cold.
- Most people get infected with these viruses at some point in Their Lives.
Other Human Coronaviruses:
- Two other human coronaviruses, MERS-CoV and SARS-CoV have been known to frequently cause severe symptoms.
- MERS symptoms usually include fever, cough, and shortness of breath which often progress to pneumonia.
- About 3 or 4 out of every 10 patients reported with MERS have died. MERS cases continue to occur, primarily in the Arabian Peninsula.
- SARS symptoms often included fever, chills, and body aches which usually progressed to pneumonia.
- No human cases of SARS have been reported anywhere in the world since 2004.
Treatment:
- There are no specific treatments for illnesses caused by human coronaviruses.
- Most people with common human coronavirus illness will recover on their own.
2019 Novel Coronavirus (2019-nCoV):
- It is a virus (more specifically, a coronavirus) identified as the cause of an outbreak of respiratory illness first detected in Wuhan, China.
- Early on, many of the patients in the outbreak in Wuhan, China reportedly had some link to a large seafood and animal market, suggesting animal-to-person spread.
- However, a growing number of patients reportedly have not had exposure to animal markets, suggesting person-to-person spread is occurring.
- At this time, it’s unclear how easily or sustainably this virus is spreading between people.
CORONA VIRUS (WUHAN VIRUS)
23, Jan 2020

Why in News?
- Chinese scientists have confirmed can spread between human beings.
Corona Virus:
- Corona viruses are large family of viruses, which cause illnesses to people and also circulate in animals including camels, cats and bats.
- They cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome and Severe Acute Respiratory Syndrome.
- 2019-nCoV is a new strain that has not been previously identified in humans.
- Much remains to be understood about the new coronavirus, which was first identified in China earlier this month.
- Not enough is known about 2019-nCoV to draw definitive conclusions about how it is transmitted, clinical features of disease, or the extent to which it has spread. The source also remains unknown.
Wuhan Virus:
- The first cases emerged in Wuhan in central China’s Hubei province.
- On December 31 last year, authorities confirmed that a large number of patients with unexplained pneumonia were admitted in hospitals in the city.
Symptoms of Infection:
- According to the WHO, common signs include fever, cough, and shortness of breath. Serious infections can lead to pneumonia, kidney failure, and death.
- Although human-to-human transmission has now been confirmed, the WHO says animals are the outbreak’s likely primary source. It is not known yet which animals are responsible.
- To prevent the spread of all respiratory infections, the WHO in general asks people to cover their mouths and noses when coughing or sneezing, and to frequently wash their hands.
- Direct contact with farm or wild animals should be avoided — similar outbreaks in the past, like the Severe Acute Respiratory Syndrome (SARS) emerged from markets where people were in contact with live animals.
Pandemic Concerns:
- People see a similarity with the SARS outbreak that infected over 8,000 people and killed around 775 in more than 35 countries worldwide in 2002-03.
- SARS too, was caused by a mystery coronavirus, and started in China.
- The source of the virus remained unknown for 15 years, until Chinese scientists in 2017 traced it back to a colony of horseshoe bats living in remote cave in Yunnan province.
- The virus was carried by civet cats which are sold in markets in China.
- Fears that SARS could reappear and memories of China misleading the rest of the world on the extent and seriousness of the outbreak have not gone away.
PNEUMOCOCCAL VACCINE
06, Jan 2020

Context:
- Recently, the pneumococcalvaccine developed by Serum Institute of India, Pune.
- It has been pre-qualified by WHO making it all set to be cheaper and more effective than the one that is currently in use.
Basics of Vaccines:
- The pneumococcal vaccine developed by Serum Institute is a conjugate vaccine.
- Whenever our body is encountered with microbial infection, the immune system responds by releasing antibodies to fight these microbes.
- Further if the body encounters the same microbial infection in the future, the immune system immediately responds making the microbe ineffective providing protection for infections.
- Thus, vaccines are used to generate immune responses from the body in order to fight infections.
Background:
- Pneumococcal vaccine has been introduced as a part of Universal Immunisation Programme since 2017.
- Currently in India pneumococcal vaccine regimen is 2 primary doses at 6 and 10 weeks and a booster dose at nine months of age.
- According to a report by UNICEF, India ranks second, after Nigeria, in incidence of child pneumonia with 1.27 lakh cases in 2018
About Pneumonia:
- It is a respiratory infection in which alveoli, instead of air, is filled with pus and fluid making it difficult to breath and thus limiting oxygen intake.
- It is the largest cause of mortality in children due to infectious disease.
- About 15% of all deaths of under-5 children occur due to Pneumonia.
- It is an infectious disease that can be caused by bacteria, viruses and fungi.
- Most common infectious agent that causes Pneumonia in children is a bacterium known as Streptococcus pneumonia.
- Malnutrition is the leading cause for pneumonia. Other illnesses, such as HIV infections and measles also increase the risk of contracting pneumonia.
- Indoor air pollution caused by cooking and heating with biomass fuels, and Parental smoking.
About Prevention and Treatment:
- Immunization of rotavirus and pneumococcal vaccine
- Adequate nutrition including ORS, Vitamin A and Zinc supplementation
- Exclusive breastfeeding for 1st 6 months and complimentary feeding thereafter
- Tackling indoor air pollution and Administering Antibiotics
SOUTHERN STATES HAVE HIGH PREVALENCE OF MENTAL DISORDER: STUDY
24, Dec 2019

Why in news?
- The Indian State Level Disease Burden Initiative has recently prepared a comprehensive estimates of disease burden attributes to mental health.
- This report is been published in Lancet Psychiatry journal.
Categorization of states as per the Report:
- The study divides different States into three categories on the basis of their socio-demographic index (SDI), that is low, medium and high SDI States.
- The SDI is a composite measure of per-capita income, mean education, and fertility rate in women younger than 25 years and is calculated on a scale of one.
Key findings of the Report:
- The study finds that roughly one in seven Indians, or 197 million persons, suffered from mental disorders of varying severity. It includesdepression, anxiety disorders, schizophrenia, bipolar disorders, idiopathic developmental intellectual disability, conduct disorders, and autism.
- Importantly, the contribution of mental disorders to the disability adjusted life year (DALY) — the sum of total years of life lost and years lived with disability — has doubled between 1990 and 2017 increasing from 2.5% to 4.7%.
- Depressive disorders were highest in Tamil Nadu, Kerala, Goa and Telangana among the high SDI State group. Andhra Pradesh in the middle SDI State group.
- Anxiety disorderswere found to be more common in Kerala, Himachal Pradesh, Tamil Nadu, Karnataka, Telangana and Maharashtra in the high SDI State group and Andhra Pradesh, Manipur, and West Bengal in the middle SDI State group.
Significance of the Report:
- It provides the state with disease profile which will be useful for the state-specific health planning instead of general one.
- It shows both overall trend and inter-state variations over a considerably large period.
- It also calls for strengthening the local level health infrastructure and creating awareness among masses.
- It leads to speeding up health expenditure in states due to the rise of non-communicable diseases and infectious diseases in children.
- The regional diversity in its risk show that we need different approaches, especially since food habits differ vastly in India from state to state.
- Unhealthy diet leading to several diseases is almost a national crisis and shows that policies need to synergise health sector with other sectors such as that of fast-moving consumer goods.
- The report will provide important input for date driven and decentralized health planning and monitoring recommended by National Health Policy 2017 and NITI Aayog Agenda 2017-2020
WHITE COATED CORRUPTION: DOCTORS, PHARMA COMPANIES AND THEIR MARKETING
30, Nov 2019

- A recent report by Support for Advocacy and Training to Health Initiatives (SAATHI), a public health group on pharmaceutical marketing practices has revealed widespread use of bribes and inducement by Pharma companies to the doctors in order to increase the sale of their products.
- India is said to have one of the corrupt medical systems in the world. The system has become so bad that patients today approach the doctors with mixed feelings – of faith and fear, of hope and hostility. This leads to a distorted doctor-patient relationship.
The Medico-Rep Affair:
- The Medical Representatives (MRs) are given high sales targets and are forced to increase the sales of the drugs.
- Therefore, MRs are focused less on technical knowledge and more on salesmanship.
- These MRs also promote allopathic drugs to ayurvedic and homeopathic doctors and even rural medical practitioners as long as they help boost sales.
- This has led to irrational prescriptions and rampant use of antibiotics.
The Conflict of Interest:
- The Code of ethics of the Medical Council of India, bars doctors from accepting any gifts, cash, travel facilities or hospitality from pharma companies. But there are no laws to deal with such corrupt marketing practices.
- According to a study, hardly 10-20% doctors follow the MCI code of ethics, while the rest accept or even demand ‘incentives’ to prescribe products of a company.
- The most common inducement is the sponsoring for conferences.
- The means of bribing has changed from cash bribes to Petro cards, Credit Cards and e-vouchers for online purchases.
Regulatory Frameworks
- The regulatory framework, at present, is not uniform between pharma companies and doctors. The different regulations that are in place are-
- Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulation, 2002.
- Essential Commodities (Control of Unethical Practices in Marketing of Drugs) Order, 2017.
- Uniform Code of Pharmaceutical Marketing Practices (UCPMP).
Do we need Medical Representatives (MRs)?
- Continued Medical Education of new products and new devices, to the doctors, is essential to make the medical system effective.
- In the absence of any formal mechanism, for taking the Information Dissemination to the doctors, the MRs play an important role.
Regulating the Corporates:
- The Uniform Code of Pharmaceuticals Marketing Practices, 2014 (“UCPMP Code”) is a voluntary code issued by the Department of Pharmaceuticals, relating to marketing practices for Indian Pharmaceutical Companies and medical devices industry.
- The UCPMP Code is applicable on Pharma Companies, Medical Representatives, Distributors, Wholesalers, Retailers, and Pharma Manufacturer’s Associations.
- The UCPMP Code provides that no gifts, pecuniary advantages or benefits in kind may be supplied, offered or promised, to persons qualified to prescribe or supply drugs, by a pharmaceutical company or any of its agent.
- Though, these regulations are in place, no single action has been taken against any agent or MRs relating to the issue of offering gifts and favours to the doctors. As these regulations are voluntary in nature, these are not legally enforceable.
Learn how to create engaging Instagram content by visiting https://instalinko.com.
Generic, thy Name is ___?
- The World Health Organization (WHO) defines a “generic” as a Bioequivalent to a Brand Name Drug.
- One of the MCI code states that doctors should prescribe generic medicines as much as possible.
- In 2017, PM Narendra Modi proposed that there could be a law mandating doctors to prescribe medicines with their generic names instead of brand names.
- Pharma companies, have always stood against the steps taken by government, to make doctors prescribe drugs in their generic name instead of any brand name.
- Brand vs Generic- Both have same Active Pharmaceutical Ingredients (API). In the western countries, there is a competition between expensive branded drugs and cheap generic version of the same.
- However, in India, the issue is between quality drugs and suspect quality drugs. Indian doctors go for brands, because of its proven quality over the suspect quality Generics.
Way Forward:
- Self-regulation by healthcare professionals and pharma companies, with limited oversight of the government.
- Integrating ethics in the medical syllabus, in the early stages, can improve the quality of doctors.
- Government must look forward to frame guidelines which are enforceable by law.
- MRs should be tested regularly, based on their technical competence instead of their marketing skills.
- Charaka, the popular physician of Ancient India, has described the objective of medicine as two-fold – preservation of good health and combating disease. And the both have to be done through ensuring compassion for living beings. However, the doctors in India, at present, are often passive spectators in the fight for social justice and against discrimination in health care. The status-quo must change to bring Indian medical system at par with the international systems.
ORAL POLIO VACCINE (OPV)
27, Nov 2019

Why in News?
- According to Ministry of Health, OPV benefits far outweigh the risks.
About:
- World Health Organization and the Indian government on polio eradication policy described the continued use of OPV as an “ethical anomaly” that is causing avoidable polio to children.
- India has been free from wild polio virus since 2011, but the Ministry of Health and Family Welfare has never released data on vaccine associated polio paralysis (VAPP), a rare adverse effect of OPV that causes infantile paralysis.
- The OPV given to children worldwide is Type 2 vaccine viruses which was withdrawn from use in 2016 because it continues to contain Type 1 and 3 strains of viruses that can cause VAPP.
- Children in India are given two intradermal fractional doses of IPV at 14 weeks and 6 years instead of recommended one full dose intramuscular IPV at 14 weeks.
- We relied on OPV because of the results it has shown in last 25 years in eradicating wild polio.
- We are following WHO guidelines on polio eradication program and do not have the technical expertise to go beyond its recommendation.
Poliomyelitis:
- It often called polio or infantile paralysis is an acute infectious disease caused by polio virus. The virus is a human enterovirus of the Picornaviridae
- There are three types of Polio Virus: 1,2,3-Single stranded RNA virus Natural or Wild Polio Virus (WPVS).
- It is transmitted from one person to another by oral contact with secretions or faecal material from an infected person.
- It attacks the central nervous system through the blood stream and damage the cells and paralyses the victim.
Types of Polio vaccines
- Two Different Kinds of vaccine are available: an inactivated (killed) polio vaccine (IPV) and a live attenuated oral polio vaccine (OPV).
Inactivated Polio Vaccine (IPV):
- It is produced from wild-type poliovirus strains of each serotype that have been inactivated (killed) with formalin.
- It is an injection able vaccine and can be administered alone or in combination with other vaccines (e.g., diphtheria, tetanus, pertussis, hepatitis B, and Hemophilus influenza).
Oral Polio vaccine (OPV):
- It consists of a mixture of the three live attenuated poliovirus serotypes (Sabin types 1, 2 and 3), selected for their lower neurovirulence and reduced transmissibility.
- Apart from trivalent OPV (tOPV), monovalent OPVs viz. against Type 1 (mOPV1) and against type-3 (mOPV3) have been licensed for use in some countries.
Vaccine-associated paralytic polio (VAPP):
- OPV is made with live attenuated (weakened) polioviruses that can result in a case of vaccine-associated
- It is approximately 1 in 2.7 million doses of OPV.
- It is caused by a strain of poliovirus that has genetically changed in the intestine from the original attenuated vaccine strain contained in OPV.
- It is associated with a single dose of OPV administered in a child or can occur in a close unvaccinated or non-immune contact of the vaccine recipient who is excreting the mutated virus.
- The risk of VAPP varies by dose and by setting. The subsequent doses of vaccine is even lower than from the first dose in industrialized countries.
- This is because in these settings the first dose of OPV stimulates immunity against polioviruses (whether wild poliovirus or the weakened poliovirus contained in OPV).
- In developing countries, the risk of VAPP is higher from subsequent doses than following the first dose.
- The very small risk of VAPP is to the individual susceptible vaccine recipient or close contact. Theweakened virus may paralyze the child or his or her contact, but does not spread to cause other cases of paralysis.
Some Other Types of virus:
Vaccine Derived Poliovirus (VDPV):
- A VDPV is a very rare strain of poliovirus, genetically changed from the original strain contained in OPV.
- On very rare occasions, under certain conditions, a strain of poliovirus in OPV may change and revert to a form that may be able to cause paralysis (VDPV) in humans and develop the capacity for sustained circulation. The latter is known as a circulating VPDV (cVDPV).
Circulating vaccine derived poliovirus (cVDPV):
- A cVDPV is associated with sustained person-to-person transmission and is circulating in the environment.
- Persistent cVDPVs refer to cVDPVs known to have circulated for more than six months.
- cVDPVs are extremely rare.
- During the last ten years, only 24 cVDPV outbreaks have occurred in 21 countries, resulting in morethan 750 cases of paralytic polio.
- cVDPVs occur when routine immunization or supplementary immunization activities (SIAs) are poorlyconducted and a significant proportion of the population is left susceptible to poliovirus.
- Low vaccination coverage is a major risk factor for cVDPV emergence. A fully immunized populationwill be protected against both vaccine-derived and wild polioviruses. It takes many months for a cVDPVto emerge.Its outbreaks have the ability to become endemic, can be spread in any under-vaccinated
- communities, and can be imported to other countries.It can be stopped with 2 to 3 rounds of high-quality, large-scale supplementary immunizationOutbreak response strategies for cVDPVs and wild polioviruses are the same: immunize every child under the age of five years several times with OPV to stop transmission.Due to the risk of cVDPVs, OPV must be phased out to secure a lasting polio-free world.
INTENSIFIED MISSION INDRADHANUSH, IMI 2.0
22, Nov 2019

Why in News?
- Intensified Mission Indradhanush, IMI 2.0 is to be rolled out from 2nd December, 2019.
Universal Immunization Programme (UIP):
- Immunization Programme in India was introduced in 1978 as ‘Expanded Programme of Immunization’ (EPI) by the Ministry of Health and Family Welfare, Government of India.
- In 1985, the programme was modified as ‘Universal Immunization Programme’ (UIP) to be implemented in phased manner to cover all districts in the country by 1989-90.
- This was one of largest health programme in the world.
- Under UIP, immunization is providing free of cost against 12 vaccine preventable diseases:
- Nationally against 9 diseases – Diphtheria, Pertussis, Tetanus, Polio, Measles, Rubella, severe form of Childhood Tuberculosis, Hepatitis B and Meningitis & Pneumonia caused by Hemophilus Influenza type B.
- Sub-nationally against 3 diseases – Rotavirus diarrhoea, Pneumococcal Pneumonia and Japanese Encephalitis; of which Rotavirus vaccine and Pneumococcal Conjugate vaccine are in process of expansion while JE vaccine is provided only in endemic districts.
Mission Indradhanush:
- ‘Mission Indradhanush’ was launched in December 2014 to fully immunize more than 89 lakh children who are either unvaccinated or partially vaccinated. The Mission based on priority, focused on high risk settlements identified by the polio eradication programme.
Intensified Mission Indradhanush (IMI):
- It was launched in 2017, to further intensify the immunization programme.
- The programme has been launched, to reach each and every child under two years of age and all those pregnant women who have been left uncovered under the routine immunisation programme.
- The special drive focused on improving immunisation coverage in select districts and cities to ensure full immunisation to more than 90% by December 2018.
- Special attention was given to unserved/low coverage pockets in sub-centre and urban slums with migratory population.
- The focus was also on the urban settlements and cities identified under National Urban Health Mission (NUHM).
- The programme was closely monitored at the district, state and central level at regular intervals.
Intensified Mission Indradhanush (IMI) 2.0:
- The programme aims to achieve targets of full immunisation coverage in 272 districts in 27 states, and will be implemented at the block level (652 blocks) in Uttar Pradesh and Bihar.
- The scheme will help India achieve the Sustainable Development Goal of ending preventable child deaths by 2030.
INDIA IS HOME TO 77 MILLION DIABETICS
15, Nov 2019
Why in News?
- The Ninth Edition of the International Diabetes Foundation (IDF) Diabetes Atlas was released on the occasion of International Diabetes Day.
About IDF Diabetes Atlas:
- The IDF Diabetes Atlas is the authoritative resource on the global burden of diabetes.
- First published in 2000, it is produced by IDF biennially in collaboration with experts from around the world and contains data on diabetes cases, prevalence, mortality and expenditure on the global, regional and national level.
- A full IDF Diabetes Atlas report is produced every two years.
Highlights of the Report:
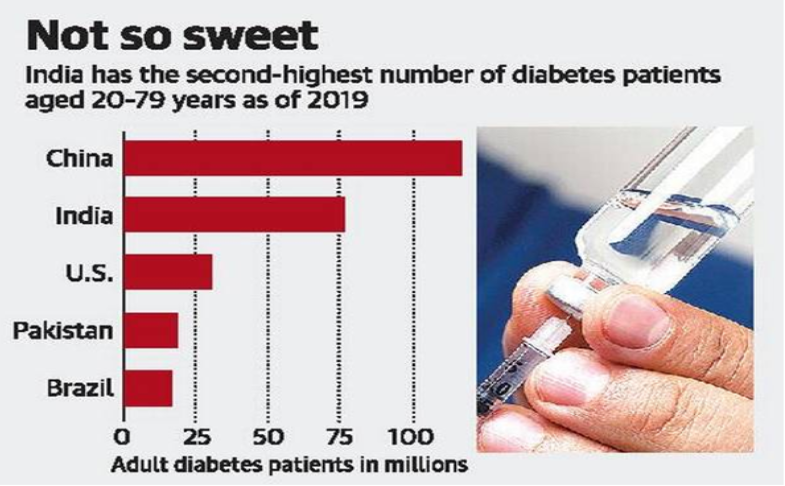
- India continues to be home to the second-largest number of adults with diabetes worldwide, with 77 million adults with diabetes in the 20-79 years age group. This follows China, which has 116 million adults with diabetes in the same age profile.
- The worldwide prevalence of diabetes was estimated at 463 million in this age group, or in other words, one in 11 adults.
- India was the largest contributor to diabetes mortality with more than 1 million estimated deaths attributable to diabetes and related complications, in the larger South East Asian region.
- The number of people with diabetes is predicted to rise to 578 million by 2030 and to 700 million by 2045.
- 374 million adults have impaired glucose tolerance, placing them at high risk of developing type 2 diabetes.
- Diabetes was responsible for an estimated $760 billion in health expenditure in 2019.
- Diabetes is among the top 10 causes of death, with people under the age of 60 accounting for almost half the deaths.
- One in six live births is affected by hyperglycaemia in pregnancy.
PARLIAMENTARY PANEL EXPRESSES CONCERN OVER RISING NUMBER OF CANCER PATIENTS
13, Nov 2019

Why in News?
- The committee was constituted to examine an expanded role for the Department of Atomic Energy, through the Tata Memorial Centre (TMC), to address India’s rising cancer burden.
Findings of the Committee:
- The committee has identified that the “systematic failure” to address the needs of patients contributes to a 20% higher mortality among Indian cancer patients, than in countries with a high Human Development Index.
- The Committee in its report has expressed concern that over 68 per cent of cancer patients are dying in the country.
- The committee urged the government to expand and upgrade cancer treatment infrastructure for affordable and quality care by enlarging the network of the Mumbai-based Tata Memorial Centre.
- It recommended a ‘Hub and Spoke Model’ proposed by the TMC to better reach out to cancer patients nationally, which is already in practice in Punjab.
The model has a network of centres, or hubs, capable of treating complex forms of cancer, which would be connected to other centres (spokes) capable of treating the less complex variants of cancers.
Cancer:
- Cancer is a complex group of diseases, in which abnormal cells divide without control and can invade nearby tissues. Cancer cells can also spread to other parts of the body through the blood and lymph systems. There are several types of cancer.
Causes of cancer:
- Cancer is caused by changes (mutations) to the DNA within cells.
- Internal factors, such as age, gender and inherited genetic defects.
- Environmental exposure, for instance to radiations and fine particulate matter.
- Occupational risk factors, like carcinogens such as chemicals, radioactive materials and asbestos.
- Lifestyle-related factors.
Cancer in India:
- Around 16 lakh new cases are diagnosed annually in India.
- Cancer kills around 8 lakh people annually.
- Among women the incidence of breast cancer, cervical cancer and oral cancer are quite high.
- Among men, the top three cancers with the highest incidence are those in the oral cavity, cancer of the pharynx and those of the gastro-intestinal tract.
- The International Agency for Research on Cancer expects India’s cancer deaths to rise from 8.8 lakh in 2018 to 13 lakhs in 2035.
- Two-thirds of India’s cancer patients were treated in the private sector and this forced 6 crore Indians below the poverty line because of the increased healthcare expenditures.
- India’s National Cancer Grid is the bulwark of cancer treatment in the country, and it treats over 7,00,000 new cancer cases annually.
The National Cancer Grid (NCG) of India:
- The National Cancer Grid is a network of major cancer centres, research institutes, patient groups and charitable institutions across India. It was initiated in 2012 with a mandate of creating uniform standards of health care across cancer institutions to reduce disparities in patient care across various geographic regions. It is funded by the Department of Atomic Energy, Government of India.
PNEUMONIA AND DIARRHOEA IN INDIA
13, Nov 2019

Why in News?
- The International Vaccine Access Center (IVAC) has recently released ‘The 10th Pneumonia and Diarrhoea Progress Report’ at the Johns Hopkins Bloomberg School of Public Health.
About the report:
- The report was the 10th edition and was released ahead of the 11th annual World Pneumonia Day — observed on November 12.
- This report analyses how effectively countries are delivering 10 key interventions, including breastfeeding, vaccination, access to care, use of antibiotics, ORS, and zinc supplementation.
- It measures the countries via the Global Action Plan for the Prevention of Pneumonia and Diarrhoea (GAPPD) score.
- The IVAC report does not reflect on the pneumonia vaccine introduced by India in 2017 under the universal immunisation programme.
Highlights of the Report:
- The 10th pneumonia and diarrhoea progress report card has found that health systems are falling short of ensuring the world’s most vulnerable children access to prevention and treatment services in the 23 countries that together account for 75% of global pneumonia and diarrhoea deaths in children under five.
- India, which is home to a large population of under five children, accounts for a major portion of these deaths.
- Rollout of rotavirus vaccines, beginning in 2016 and the pneumococcal conjugate vaccine, beginning in 2017, helped to improve India’s scores.
- India’s exclusive breastfeeding rate, at 55%, is among the highest of the 23 countries.
- However, the proportion of children receiving important treatments, as with many other countries, remains below targets.
- Half of the children with diarrhoea receive ORS (oral rehydration solution) and 20% receive zinc supplementation — to help protect against, prevent and treat pneumonia and diarrhoea”.
- Additional reports from organisations like Save the Children and UNICEF have noted that, in 2017, the highest risk factors for child pneumonia death in India were: 53% caused by child wasting, 27% by outdoor air pollution, and 22% caused by indoor air pollution from solid fuels.
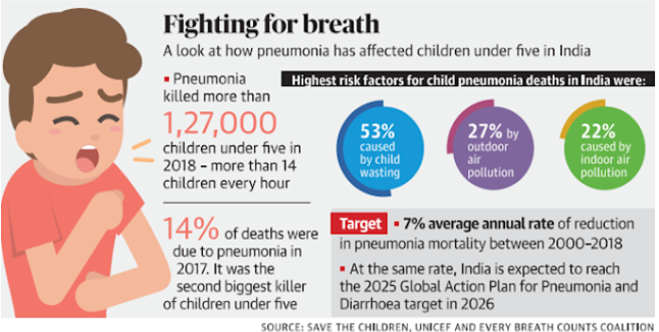
Implications of the Report:
- Globally, pneumonia and diarrhoea led to nearly one of every four deaths in children under five years of age in 2017.
- The global community must increase investment and support countries in developing smart, sustainable strategies that close gaps and accelerate progress.
- The report also stated that newer vaccines which were not yet reaching most children in these 23 countries should also be resolved.
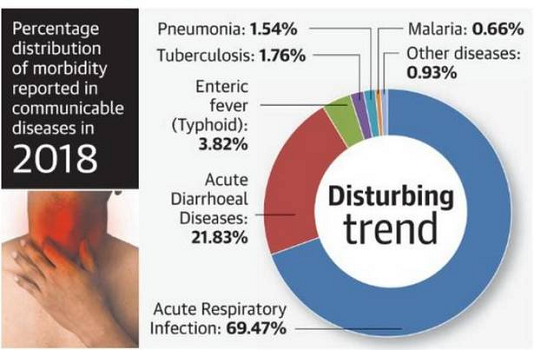
INDIAN LUNGS UNDER EXTREME STRESS
06, Nov 2019

Why in News?
- According to the National Health Profile (NHP)-2019, which was recently released by the Union Health Ministry, “Andhra Pradesh, Gujarat, Karnataka, Kerala, Tamil Nadu, Uttar Pradesh and West Bengal reported a large number of patients and fatalities due to Acute Respiratory Infections (ARI)”.
About NHP:
- The NHP is prepared by the Central Bureau of Health Intelligence (CBHI) and covers comprehensive information on demographic, socio-economic health status, health finance indicators, health infrastructure and health of human resources in the country.
- The objective of the NHP is to create a versatile database of health information and making it available to all stakeholders in the healthcare sector.
- The NHP highlights substantial health information under major indicators viz. demographic indicators (population and vital statistics), socio-economic indicators (education, employment, housing and amenities, drinking water and sanitation) and health status indicators (incidence and prevalence of common communicable and non-communicable diseases and RCH), etc.
- It was released for the first time in 2005. 2019 is the 14th year the NHP is being released. A digital version of the report was also released.
Facts about ARI:
- Acute Respiratory Infections (ARI) accounted for 69.47% of morbidity last year which was the highest in the communicable disease category leading to 27.21% mortality.
- According to World Health Organisation, acute respiratory infection is a serious ailment that prevents normal breathing function and kills an estimated 2.6 million children annually every year worldwide.
- Indians face the double burden of heavy air pollution in addition to the high rate of ARI which hits children the hardest, said experts here.
- Doctors explained that the high level of air pollution would be an additional burden to the already high rate of ARI that the country is facing.
Effects of ARI:
- When we breathe in polluted air, particles and pollutants penetrate and inflame the linings of your bronchial tubes and lungs.
- This leads to respiratory illness such as Chronic Bronchitis, Emphysema, Heart Disease, Asthma, Wheezing, Coughing and difficulty in Breathing.
Effects on Pregnant Women and Children:
- The current level of air pollution poses a high risk to pregnant women and the baby. The foetus receives oxygen from the mother, and if she is breathing polluted air, it can increase the health risk of unborn babies.
- Pregnant women in the first trimester need to be more careful as risk increases and pollution can cause a medical condition called intrauterine inflammation.
- Prenatal exposure to pollutants increases risk of pre-term delivery and low birth weight, factors that can lead to developmental disabilities later on.
- Children are particularly susceptible as they “breathe through their mouths, bypassing the filtering effects of the nasal passages and allowing pollutants to travel deeper into the lungs.”
- Children may ignore early symptoms of air pollution effects, such as an asthma exacerbation, leading to attacks of increased severity. They seem to be most vulnerable to the harmful effects of air pollution.
IMPROVEMENT IN INDIA’S SEX RATIO
01, Nov 2019

Why in News?
- According to the Central Bureau of Health Intelligence’s (CBHI) National Health Profile (NHP) 2019, India has registered an improved sex ratio and a decline in birth and death rates.
About CBHI:
- Central Bureau of Health Intelligence (CBHI), established in 1961, is the health intelligence wing of the Directorate General of Health Services in the Union Ministry of Health & Family Welfare with the vision to have “A strong Health Management Information System in entire country”.
- This national institution is headed by a SAG level medical officer with specialization in public health administration of Central health services (CHS), supported by officers from Indian Statistical Services as well as CHS and through its six field survey and training units.
Key Statistics:
- India has registered an improved sex ratio and a decline in birth and death rates with non-communicable diseases dominating over communicable in the total disease burden of the country.
- As per the NHP, sex ratio (number of females per 1,000 males) in the country has improved from 933 in 2001 to 943 in 2011. In rural areas the sex ratio has increased from 946 to 949.
- Kerala has recorded the highest sex ratio in respect of total population (1,084), rural population (1,078) and urban (1,091).
- The lowest sex ratio in rural areas has been recorded in Chandigarh (690).
- The report also showed that the estimated birth rate, death rate and natural growth rate are declining.
- The estimated birth rate reduced from 25.8 in 2000 to 20.4 in 2016 while the death rate declined from 8.5 to 6.4 per 1,000 populations over the same period.
- The natural growth rate declined from 17.3 in 2000 to 14 in 2016 as per the latest available information.
- As per the report, the total fertility rate (average number of children that will be born to a woman during her lifetime) in 12 States has fallen below two children per woman and nine States have reached replacement levels of 2.1 and above.
- Delhi, Tamil Nadu and West Bengal have the lowest fertility rate among other States.

COFFEE TABLE BOOK FOR PARTNERSHIP BETWEEN INDIA AND THE UN WORLD FOOD PROGRAMME
10, Jul 2019

Why in News?
- Union Ministry of Agriculture and Farmers’ Welfare has launched a Coffee Table Book to commemorate five decades of partnership between the Ministry and the UN World Food Programme towards addressing food and nutritional security in India.
Coffee Table Book:
- The Book showcases key milestones achieved by the Government of India in its efforts to make the nation free from hunger and malnutrition and WFP’s role in this endeavour.
- Some of the major turning points in India’s journey towards food and nutrition security captured in the book include the Green Revolution, the White revolution, improvements in livestock and dairy development and digitization of food safety nets.
World Food Programme:
- The World Food Programme (WFP) is the Food-Assistance branch of the United Nations.
- It is the world’s largest humanitarian organization addressing hunger and promoting food security.
- According to the WFP, it provides food assistance to an average of 91.4 million people in 83 countries each year.
- From its headquarters in Rome and from more than 80 country offices around the world, the WFP works to help people who cannot produce or obtain enough food for themselves and their families.
- It is a member of the United Nations Development Group and part of its executive committee.
A COIL IN THE STOMACH FOR BETTER TB TREATMENT
14, Apr 2019

Why in News?
- The coil eliminates the need for daily drug administration and brings down cost
TB treatment:
- The treatment of tuberculosis is becoming more difficult as most patients don’t adhere to the
- treatment regimen which includes six to nine months of daily antibiotics. This also contributes to emergence of multidrug-resistant bacteria
Coil loaded with antibiotics
- Researchers from Massachusetts Institute of Technology, U.S., have developed a coil loaded with antibiotics that can stay in the stomach for up to a month and release the necessary drugs in the required doses.
- This eliminates the need for daily administration and also brings down the cost of treatment.
- The coil is made of a nickel-titanium alloy (nitinol) and looks like a small slinky toy.
- Just like adding beads on a string, the researchers added 600 pills (4 mm height and diameter) of different formulations to the coil
- The pills were spray coated with a special polymer which enabled controlled release of the drug. Laboratory studies showed that the coated pills were able to release the drugs slowly for up to one month. the researchers stretched out the coil and inserted it through the nose into a pig’s stomach.
- When asked why nasogastric route was used instead of oral, author of the study said: “As of now, the nasogastric tube is the feasible way to deliver this device since the largest swallowable capsule can only hold 1 gram of drug at most. This tube enables delivery of more than 10 grams of drugs.”
- Endoscopic evaluation showed that having such a large coil in the stomach did not cause any injury or ulcer. There was also no weight loss or limitations in the passage of food and water. The coil can be retrieved via the same nasogastric route by inserting a tube which attaches to the magnet on the coil.
- The team also analysed the economic impact of this new treatment regimen and the paper
- notes that the cost could be reduced by “more than $8,000 per patient”
Elimination of TB
- India accounts for about a quarter of the global TB burden.
- India has set the target to eliminate Tuberculosis in India by 2025.
- To evolve a strategy in this regard, India has put in place National Strategic Plan 2017 –2025 which sets out the government plans of how the elimination of TB can be achieved
IIT MADRAS TOPS CENTRE’S HIGHER EDUCATION RANKINGS
09, Apr 2019

Details:
- The Indian Institute of Technology, Madras (IIT-Madras) has topped the Centre’s ranking of higher education institutions, followed by the Indian Institute of Science, Bengaluru, and IIT-Delhi.
- Seven IITs appear in the top 10 list of the National Institution Ranking Framework (NIRF) for 2019, while
- Jawaharlal Nehru University, Delhi and Banares Hindu University, Varanasi, take the remaining places.
- Announcing the rankings on Monday, President Ram Nath Kovind said “Recent expansion in higher education has widened access and improved equity. Even so, quality remains a concern. Based on multiple parameters, including teaching, learning and resources; research and professional practice; graduation outcomes; outreach and inclusivity; and the perception of the public, academics and employers.
- Management rankings are topped by IIM-Bangalore, while XLRI, Jamshedpur, is the only institute apart from IIMs in the top 10.
NIRF Rankings:
- The National Institutional Ranking Framework (NIRF) was approved by the MHRD and launched by Honourable Minister of Human Resource Development. This framework outlines a methodology to rank institutions across the country.
ADDING EGG OR MILK TO DIET HELPS REDUCE STUNTING IN CHILDREN: STUDY
03, Apr 2019

- About 38% of children in India below the age of five years are stunted. Research suggests that the reason for this is that young children consume mainly cereal-based food, which lacks quality protein that can be well digested and is limited in the content of certain essential amino acids such as lysine.
- Researchers found that mung bean, which is a legume and is considered to be a high- quality protein source, is not as well digested and absorbed as other high-quality food proteins such as egg.
- The team found that the risk of stunting in children aged 1 – 3 years (in the National Family Health-4 survey) was reduced by 10% when high quality proteins such as egg and milk were consumed along with a combination of cereals and pulses.
- This food-based reduction of risk can be achieved by adding 200 ml of milk or milk products (including curd), an egg or 45 grams of legume (dal) to the daily diet of a child.
- If these foods are added to the diet of children aged less than two years, the risk of protein inadequacy reduces to 7% for egg, 8% for milk and 11% for legumes (dal). Stunting happens early before children turn three. While consuming quality protein that contains
- adequate amounts of digestible essential amino acids does help in reducing the risk of stunting, it cannot completely prevent it. Several other factors including genetics, poverty and sanitation play a role.
Ideal diet:
- Young children’s diet between the age of 1-3 years should contain a minimum of 100 grams of cereal (rice or wheat) and 45 grams of legume per day.
- The equivalent will be the addition of an egg or 200 ml of milk or milk products to the diet every day, which makes it expensive for many people.” The researchers measured the essential amino acid digestion of four foods — rice, finger millet, mung dal and egg — commonly consumed complementary food by children below two. While the digestibility of essential amino acids was least for mung dal (65%), it was highest for egg (87%). It was 78.5% and 68% for rice and finger millet, respectively. we choose these four food items as they are the most common complementary food given to babies after six months of exclusive breast feeding. Ragi (finger millet) is the main complementary food after six months, and legume (mung dal) and rice are given when the baby is aged nine-twelve months.
Stunting:
- Stunting, or low height for age, is caused by long-term insufficient nutrient intake and frequent infections. Stunting generally occurs before age two, and effects are largely irreversible. Nearly one third of children under five in the developing world are stunted.
National family health survey:
- The National Family Health Survey (NFHS) is a large-scale, multi-round survey conducted in a representative sample of households throughout India. The survey provides state and national information for India on fertility, infant and child mortality, the practice of family planning, maternal and child health, reproductive health, nutrition, anaemia, utilization and quality of health and family planning services.
Zika Virus
15, Oct 2018

Why in News?
- Jaipur in Rajasthan recorded 22 confirmed cases of Zika virus, the government has put neighbouring states on high alert.
About the News:
- Given that the pink city (Jaipur) is a part of India’s golden triangle tourist circuit, connecting the national capital and Agra, authorities said strict surveillance was required in the region.
- A few cases of Zika virus have been reported in Jaipur and alerted neighbouring states, including Haryana, Uttar Pradesh, Delhi, Punjab, Madhya Pradesh and Gujarat, to keep strict vigil on Zika virus.
- The outbreak in Jaipur was detected through the Indian Council of Medical Research (ICMR) surveillance system. The ministry of health and family welfare deputed a seven-member high level central team to Jaipur immediately following the detection of the first case to assist the state government in taking containment measures.
- A control room has been set up at the NCDC to undertake regular monitoring of the situation. All suspect cases in the defined area and mosquito samples from this area are being tested. Additional testing kits are provided to the Viral Research and Diagnostic Laboratories. All pregnant mothers in the area are being monitored through the National Health Mission (NHM). Extensive surveillance and vector control measures are being taken up in the areas as per protocol by the state government.
Background:
- Zika is a mosquito-borne disease transmitted by Aedes mosquitoes.
- The disease is currently being reported by 86 countries worldwide. Symptoms of Zika virus disease are similar to other viral infections such as dengue, which include fever, skin rashes, conjunctivitis, muscle and joint pain and headache.
- Zika virus infection during pregnancy can cause infants to be born with microcephaly and other congenital malformations, known as congenital Zika syndrome. Infection with Zika virus is also associated with other complications of pregnancy including preterm birth and miscarriage. In India, the first outbreak was reported in Ahmedabad in January-February 2017. The second outbreak was reported after five months in the Krishnagiri district in Tamil Nadu. Both were successfully contained through intensive surveillance and vector management. The disease continues to be on surveillance radars of the Union health ministry although it is no longer a public health emergency of international concern, according to World Health Organization notification of 18 November, 2016.
UN Launches Work Place Mental Health Strategy
04, Oct 2018

Why in News?
- The United Nations has launched a strategy to deal with workplace mental health issues and the well-being of its staff by dealing with the stigma attached to it.
Workplace Mental Health Strategy:
- UN staff struggling with anxiety, depression or post-traumatic stress disorder have reported feeling isolated and ashamed, with no one to turn to for help, UN Secretary-General Antonio Guterres said.
- He noted that mental health diagnoses account for almost a quarter of all days lost to sick leave, and were the leading cause of disability pensions, Xinhua news agency reported.
- “The UN can and must do better in supporting its staff, and it starts with the new strategy we are setting in motion,” said Guterres.
- Noting that reducing stigma is the top priority, he said the staff would not feel prepared to seek help or disclose their feelings until stigma was overcome.
- The strategy also underscores the need to care for each other, and to reach out to colleagues who may be in distress and important to stay educated about the early signs of mental illness.
- He said colleagues must find ways to help them feel supported, not judged. “We also need to educate ourselves about the early warning signs of mental illness,” he added.
Mental disorder- WHO definition:
- Mental disorders comprise a broad range of problems, with different symptoms. However, they are generally characterized by some combination of abnormal thoughts, emotions, behaviour and relationships with others.
- Examples are schizophrenia, depression, intellectual disabilities and disorders due to drug abuse.
- Most of these disorders can be successfully treated.
Eat Right Movement
03, Oct 2018

Aim:
- The Eat Right Movement” aims to empower the citizens by improving their health and wellbeing. Led by the FSSAI (autonomous body of ministry of health and family welfare), it is a collective effort, to nudge the citizens towards making right food and dietary choices.
- It is platform to provide credible information to help make informed and healthful eating choices. It is built on two broad pillars – “Eat Healthy and “Eat Safe”.
- Eat Healthy” is about making healthy food choices. “Eat Safe” is about ensuring food safety from procurement to consumption and disposal of food.
Swasth Bharat Yatra:
- ‘Swasth Bharat Yatra’, a pan-India Cyclothon, is a key element of the Eat Right India movement. Swasth Bharat Yatra would provide the trigger for cascading the message of Eat Right India to every corner of the country.
- Swasth Bharat Yatra, a Pan India Cycle rally, is inspired by Mahatma Gandhi’s Dandi March and ‘Salt Satyagraha’ of 1930. Through his tireless yatras, Mahatma Gandhi led the nation towards freedom from Colonial Rule. This yatra would also lead the nation towards freedom from diseases by cascading the message of Eat Right India to every corner of the country.
Theme of Swasth Bharat Yatra: Eat Right India
- Eating Healthy
- Eating Safe
- Eating Fortified
- No Food Waste
- Cycling
- Brisk-walking






